II. Indications
- Pulmonary Embolism
-
Deep Vein Thrombosis (DVT)
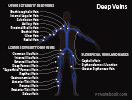
- Upper Extremity Deep Vein Thrombosis
- Brachiocephalic Vein
- Internal Jugular Vein
- Subclavian Vein
- Axillary Vein
- Basilic Vein (proximal aspect)
- Brachial Vein
- Ulnar Vein
- Radial Vein
- Lower Extremity Deep Vein Thrombosis
- Common Iliac Vein
- Internal Iliac Vein
- External Iliac Vein
- Deep Femoral Vein
- Femoral Vein ("Superficial" Femoral Vein)
- Popliteal Vein
- Gastrocnemius Vein (branch of popliteal vein)
- Anterior Tibial Vein
- Peroneal Vein
- Posterior Tibial Vein
- Soleus Vein (branch of Posterior Tibial Vein)
-
Superficial Venous Thrombosis
- Proximal superficial clot (upper thigh) especially within 5 cm of deep system or
- Clot >7 cm long in leg (or 5 cm long in arm) or
- Known clotting disorder or
- Lack of improvement after 1 week
III. Precautions: CHEST - DVT (without PE) Medication Selection Guidelines 2021
- Distal lower extremity DVT (calf DVT below the popliteal vein)
- Perform serial Ultrasound without Anticoagulation (weekly for 2 weeks)
- Indications to start Anticoagulation
- DVT extension into proximal leg veins
- Distal DVT progression on serial Ultrasound
- Proximal DVT
- Initiate Anticoagulation
-
Antiphospholipid Antibody Syndrome
- Treat with Vitamin K Antagonist (Warfarin) instead of DOAC
- Pregnancy
- Treat with Low Molecular Weight Heparin
- Active Cancer
- Direct Oral Anticoagulants (DOACs) are now recommended instead of LMWH
- Low Molecular Weight Heparin had previously been recommended
- References
IV. Management: Disposition
-
Pulmonary Embolism
- See Pulmonary Embolism
- Inpatient (typical) or if criteria met, outpatient Anticoagulation
- See Pulmonary Embolism Management for disposition criteria
- Consider risk scoring systems to assist with disposition
- Pulmonary Embolism Severity Index (PESI) Score <66 (Class 1)
- As of 2015, PESI <86 (low risk) may be reasonable for discharge
- Hestia Criteria negative
- See Hestia Criteria
- Bova Score stage 1 (low risk)
- Simplified PESI (sPESI) with no positive criteria (score 0)
- Pulmonary Embolism Severity Index (PESI) Score <66 (Class 1)
-
Deep Vein Thrombosis
- See Deep Vein Thrombosis
- Outpatient management in most cases
V. Labs
- Initial labs
- Complete Blood Count
- Polycythemia, Thrombocytosis,associated with Splenomegaly (myeloproliferative disorder)
- ProTime (INR)
- Partial Thromboplastin Time (PTT)
- Increased PTT without correction by 1:1 dilution with normal plasma
- Seen with Lupus Anticoagulant syndrome
- Increased PTT without correction by 1:1 dilution with normal plasma
- Comprehensive metabolic panel (Liver Function Tests and Renal Function tests)
- Anticoagulant doses may require adjustment
- Complete Blood Count
-
Thrombophilia work-up in idiopathic or recurrent DVT
- See Thrombophilia
- Test only if results will direct therapy (especially duration of Anticoagulation)
- Reserve blood for tests prior to Anticoagulation
- Other testing to consider
- Urinalysis
- Proteinuria (e.g. Nephrotic Syndrome)
- Hematuria (e.g. cancer)
- Chest XRay
- Consider at time of initial diagnosis if chest CT was not done
- May indicate underlying malignancy
- Urinalysis
VI. Medications: Initial Phase - Unstable Protocol with Unfractionated Heparin
-
Unfractionated Heparin (weight based Heparin)
- Goal: PTT 1.5-2.5x normal
- Allows for invasive management in case of decompensation
- Preferred in submassive PE
- In high risk patients, consider initiating Heparin while awaiting definitive imaging
VII. Medications: Initial Phase - Concomitant Protocol With Heparin
- Indications for concurrent Heparin Use (agents other than Rivaroxaban or Apixaban)
- Standard Heparin
- See Weight based Heparin nomogram for dosing
- Indications
- Severe Renal Insufficiency
- High risk of bleeding
- Hemodynamic instability
- Morbid Obesity
-
Low Molecular Weight Heparin (LMWH)
- See Low Molecular Weight Heparin for dosing
- Efficacy
- Equivalent to standard Heparin in non-massive PE
- Enoxaparin (Lovenox) 1 mg/kg twice daily
- Avoid single dose of 1.5 mg/kg daily (not recommended due to lower efficacy)
- Tinzaparin (Innohep) 175 anti-Xa IU per kg daily
- Dose (ml): (weight in kg) x 0.00875 ml/kg daily
VIII. Medications: Initial Phase - Single agent DOACs that do not require concurrent Heparin
- See Warfarin alternatives in section below
-
Rivaroxaban (Xarelto) was FDA approved for acute DVT management in Nov 2012
- As effective and safe as LMWH (see Rivaroxaban for references)
- Initial: 15 mg orally twice daily for 21 days
- Maintenance: 20 mg orally daily
- Prevention of recurrence: 20 mg orally daily
-
Apixaban (Eliquis)
- Initial: 10 mg orally twice daily for 7 days
- Maintenance: 5 mg orally twice daily
- Prevention of recurrence: 2.5 mg orally twice daily
IX. Medications: Warfarin Initiation
- See Warfarin alternatives below (Rivaroxaban, Apixiban, Dabigatran)
- Start Warfarin (Coumadin) concurrent with LMWH
-
Warfarin and DOACs are contraindicated in pregnancy, severe liver disease, Breakthrough VTE, some cancers
- See DVT in Pregnancy
- Continue Low Molecular Weight Heparin in these cases
- Initial Warfarin Dosing
- See Warfarin for further dosing information
- Age <65 years: Start 10 mg daily
- Dose of 10 mg start was therapeutic 1.4 days earlier
- Kovacs (2003) Ann Intern Med 138:714-9 [PubMed]
- Age >65 years: Start 5 mg daily
- Age >75 years: Start 2.5 mg daily
- Check INR starting in 3 days
- Therapeutic INR: 2.0 to 3.0 IU
- Continue Heparin for a minimum of 5 days AND until INR is therapeutic
X. Medications: Warfarin alternatives (Direct Oral Anticoagulants or DOACs)
- Precautions
- Avoid in pregnancy and Lactation (not studied, effects are unknown)
- See DVT in Pregnancy
- Avoid if poor adherence (DOAC levels fall subtheraputic even after a single missed dose)
- Avoid in those with Mechanical Heart Valves
- Rivaroxaban (Xarelto) and Apixiban (Eliquis) are being used for DVT in cancer as of 2020
- Avoid if GFR <30 (use Warfarin instead) or if high risk of bleeding (e.g. gastrointestinal cancer)
- Previously only Low Molecular Weight Heparin (LMWH) and Warfarin were used in cancer
- (2020) Presc Lett 27(6): 32-3
- Streiff (2018) J NatlCompr Canc Netw 16(11): 1289-303 [PubMed]
- Avoid in significant Renal Insufficiency (e.g. GFR <30 ml/min), esp. in underweight or over age 75 years old
- See specific agents for allowable GFR
- Indications (FDA approved as of 2012)
- VTE Prophylaxis
- DVT acute management (in place of LMWH) - see above
- DVT Anticoagulation
- PE Anticoagulation (not yet mainstream usage in PE)
- No adverse events when 106 low risk PE patients discharged on Rivaroxaban
- Preparations: No Heparin pretreatment needed (see above)
- Rivaroxaban (Xarelto)
- Oral Factor Xa Inhibitor that was FDA approved for acute DVT management in Nov 2012
- Rivaroxaban was found as effective and safe as LMWH (see Xarelto for references)
- See dosing above
- Apixiban (Eliquis)
- See dosing above
- Rivaroxaban (Xarelto)
- Preparations: Requires concurrent Heparin for first 5-10 days
- Edoxaban (Savaysa)
- Dosing: 60 mg orally daily (adults >60 kg)
- Dabigatran (Pradaxa)
- Initial
- Dabigatran (Pradaxa) 150 mg orally twice daily AND
- Low Molecular Weight Heparin (LMWH) or standard Heparin for 5-10 days while starting Pradaxa
- Maintenance: 150 mg orally twice daily
- Prevention of Recurrence: 150 mg orally twice daily
- Initial
- Edoxaban (Savaysa)
XI. Management: Duration of Anticoagulation
- See Thromboembolic Disease in Pregnancy
-
Anticoagulation duration has undergone significant changes since 2010
- Prior 6-12 month Anticoagulation courses have dropped to 3 month recommendations in most cases
- Most difficult decision is determining who needs longterm therapy to prevent recurrence
- Those with transient causes (e.g. surgery, Trauma) are at low risk
- Thorough history and exam is paramount in determining if Thrombophilia risk exists
- Focus on idiopathic cases
- Test only those where history and exam indicates
- D-Dimer protocol below may assist in risk stratifying idiopathic VTE and risk of recurrence
- Very low risk: 6-12 weeks
- Symptomatic isolated calf vein thrombosis
- Low risk patient: 3 months
- Reversible Venous Thromboembolism Risk (transient risk such as post-operative event) or
- Upper extremity Deep Vein Thrombosis
- Low to Moderate risk patient: At least 3 months (and consider for life-long Anticoagulation)
- First idiopathic distal DVT
- First idiopathic Pulmonary Embolism
- Moderate to high risk patient: Longterm therapy
- See Recurrent Thromboembolism Risks
- Indications
- First idiopathic proximal DVT or PE
- Recurrent idiopathic DVT or PE
- Thrombophilia
- Protocol for reduced DOAC dosing in moderate risk patients on longterm Anticoagulation
- Consider switching to lower dose DOAC after 6 months of standard therapy
- Continue Warfarin at standard dose for Prosthetic Heart Valves or severe Renal Insufficiency
- Example doses:
- Eliquis (Apixaban) 5 mg twice daily decreased to 2.5 mg twice daily
- Xarelto (Rivaroxaban) 20 mg daily decreased to 10 mg daily
- Do not low dose of Dabigatran or Edoxaban (insufficient evidence)
- References
- (2017) Presc Lett 24(6): 31
- Consider switching to lower dose DOAC after 6 months of standard therapy
- High risk patient: Low Molecular Weight Heparin or LMWH (e.g. Lovenox)
- Active cancer (continue therapy while cancer active or receiving cancer therapy)
- As of 2020, Apixaban and Rivaroxaban are being used for DVT in active cancer (see above)
- Active cancer (continue therapy while cancer active or receiving cancer therapy)
XII. Management: Recurrent VTE on Warfarin or DOAC (Breakthrough VTE)
- Epidemiology
- Breakthrough VTE occurs in 2-3% of VTE cases over a 6 month period
- Definition of Breakthrough VTE
- Recurrence despite therapeutic on Anticoagulation for at least 2 weeks
- Pulmonary Embolism is an increased risk in the first 2 weeks after DVT diagnosis and Anticoagulation start
- DVT extension occurs in the first 2 weeks in up to 30% of patients despite Anticoagulation
- Evaluate for compliance
- Has patient been consistently therapeutic?
- Have agents been taken consistently and correctly (e.g. Rivaroxaban needs to be taken with food)?
- Consider other causes of symptoms
- Post-DVT swelling and pain
- Post-Thrombotic Syndrome
- Differentiate acute new or progressive Deep Vein Thrombosis (DVT) from chronic, residual DVT
- Post-PE Shortness of Breath, Chest Pain and reduced Exercise tolerance
- Post-Pulmonary Embolism Syndrome (50% of patients at 6 months)
- Evaluate for timing of symptoms (new or old)
- Negative D-Dimer makes new Pulmonary Embolism unlikely
- Post-DVT swelling and pain
- Evaluate for underlying cause of strong Thrombophilia
- Cancer
- Severe Antiphospholipid Antibody Syndrome (or other Vasculitis)
- Also consider in patients on DOAC with Breakthrough VTE
- Consider Drug Interactions
- See Warfarin Drug Interactions
- Consider Direct Acting Anticoagulant (DOAC) interactions (CYP3A4, P-Glycoprotein)
- Evaluate for Warfarin resistance
- Consider Heparin Induced Thrombocytopenia
- Consider in those on Heparin
- Management
- Consult hematology
- Change to LMWH (e.g. Lovenox) for 3-6 months (preferred strategy)
- Other options
- Consider switching from DOAC to Warfarin (allowing for monitoring of INR) or
- Increase Warfarin dose to target higher INR (e.g. 3 to 3.5)
- Avoid IVC Filter unless Anticoagulation is contraindicated in the face of a large PE or proximal DVT
- References
- DeLoughery in Swadron (2022) EM:Rap 22(5):19-20
- Osinbowale (2009) Cleve Clin J Med 76(12): 724-30 [PubMed]
XIII. Management: Risk Stratification in Idiopathic Unprovoked first VTE
- Precautions
- American Society of Hematology recommends longterm Anticoagulation for unprovoked VTE
- Consider HERDOO2 Model for Risk Stratification in women after first unprovoked VTE
- https://www.mdcalc.com/herdoo2-rule-discontinuing-anticoagulation-unprovoked-vte
- Male gender alone is a risk for recurrent VTE (RR 1.8 in unprovoked VTE)
- Balance the risk of recurrent VTE with the risk of serious bleeding on chronic Anticoagulation
-
D-Dimer after 3 months of Anticoagulation
- D-Dimer checked 4 weeks after stopping Anticoagulation
- Recurrent DVT is lower risk if D-Dimer is negative (3%/year contrasted with 9-10%/year if positive)
- (2006) NEJM 355:1780-9 [PubMed]
- Verhovsek (2008) Ann Intern Med 149(7): 481-90 [PubMed]
- D-Dimer protocol not recommended by ACCP
- D-Dimer checked 4 weeks after stopping Anticoagulation
-
Ultrasound affected extremity at 3 months of Anticoagulation
- Recurrent DVT is low risk if residual thrombus <40%
- However, other studies suggest that residual venous Occlusion is not a risk for recurrent VTE
- (2008) Blood 112:511-5 [PubMed]
- Cosmi (2010) Eur J Vasc Endovasc Surg 39(3): 356-65 [PubMed]
- Consider Aspirin
- Indications: Unprovoked VTE (idiopathic) who are not continuing Anticoagulation after initial VTE management
- Efficacy: Number Needed to Treat (NNT) 33 to prevent one event per year
- Dose: Aspirin 81 mg orally daily
- Brighton (2012) N Engl J Med 367:1979-87 [PubMed]
XIV. Prevention
- See Deep Vein Thrombosis Prevention
- See DVT Prevention in Travelers
- See VTE Prophylaxis in Pregnancy
- Longterm Anticoagulation
- Indicated as secondary prevention of VTE as indicated above (e.g. recurrent unprovoked VTE, Thrombophilia)
-
Aspirin or other Antiplatelet Therapy
- Consider in unprovoked DVT or PE in patients who choose to discontinue Anticoagulation after initial therapy (see above)
- Suspend Aspirin or other Antiplatelet Therapy in stable cardiovascular disease while on VTE Anticoagulation
- Continue Aspirin and other antiplatelet agents only if clear indications (e.g. recent coronary stenting, Claudication)
- Otherwise, antiplatelet agents with Anticoagulation add significant bleeding risk without significant benefit
- Flumignan (2022) Cochrane Database Syst Rev (7): CD012369 [PubMed]
XV. References
- (2014) Presc Lett 21(11): 61
- DeLoughery and Orman in Majoewsky (2012) EM:Rap 12(12): 4-5
- Jean-Louis and Sethuraman (2023) Crit Dec Emerg Med 37(7): 4-11
- Hyers (2001) Chest 119:176S-93S [PubMed]
- Galioto (2011) Am Fam Physician 83(3): 293-300 [PubMed]
- Nasir (2025) Am Fam Physician 112(4): 424-34 [PubMed]
- Wigle (2019) Am Fam Physician 100(7): 426-34 [PubMed]
- Wilbur (2017) Am Fam Physician 95(5): 295-302 [PubMed]
