II. Epidemiology
- Superficial Venous Thrombosis accounts for 5% of VTE
III. Pathophysiology
- Superficial Venous Thrombosis has the similar risk factors as Venous Thromboembolism (e.g. Virchow's Triad)
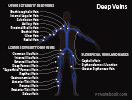
- Distribution
- Lower extremity (most common)
- Greater saphenous vein accounts for more than half of events
- Upper Extremity
- See Upper Extremity DVT
- Consider Thoracic Outlet Syndrome in unprovoked upper extremity Superficial Thrombophlebitis
- Lower extremity (most common)
IV. Signs
- Red, tender, warm inflamed region that follows the course of a vein
- Vein may be palpable
- Limb edema
V. Imaging
- Images
-
Doppler Ultrasound
- DVT identified in 25% at time of Superficial Venous Thrombosis diagnosis
- DVT identified in 10% at 3 months after Superficial Venous Thrombosis diagnosis
- Decousus (2010) Ann Intern Med 152:218-24 [PubMed]
VI. Differential Diagnosis
- Deep Vein Thrombosis
- Septic Superficial Thrombophlebitis
- Cellulitis
- Vasculitis
- Venous Insufficiency
- Ascending Lymphangitis
VII. Management: General
- Hot packs locally applied to Thrombophlebitis
-
NSAIDs (e.g. Ibuprofen)
- Contraindicated in Anticoagulation
VIII. Management: Anticoagulation
- Indications
- Proximal superficial clot (upper thigh) especially within 5 cm of deep system or
- Clot >7 cm long in leg (or 5 cm long in arm) or
- Known clotting disorder or
- Lack of improvement after 1 week
- Precautions
- Thrombus within 3 cm of sphenofemoral junction (greater saphenous vein junction with femoral vein)
- Full dose VTE Anticoagulation for 3 months is recommended
- Decision to anticoagulate is nuanced and largely based on expert opinion
- Consider local Consultation with hematology
- Decision to anticoagulate and its duration is based on multiple factors
- Upper or lower extremity
- Provoked (e.g. IV) or unprovoked
- Clot length and distance to proximal end
- Symptoms
- Hypercoagulable State
- Thrombus within 3 cm of sphenofemoral junction (greater saphenous vein junction with femoral vein)
- Management
- Rivaroxaban 10 mg orally daily
- LMWH (e.g. Lovenox) 40 mg daily or
- Fondaparinux 2.5 mg daily or
- Dalteparin 5000 IU daily
- Course
- Duration: 14 to 45 days
- Expert opinion appears to favor 45 day course
- Exceptions
- Full dose VTE Anticoagulation for 3 months if Thrombus within 3 cm of sphenofemoral junction
- Original recommendations were for 14 days
- However, short durations may be too brief to prevent progression or recurrence
- Indications to extend course to longer duration (30 to 45 days)
- Persistently inflamed (red, painful) or
- Close proximity to perforators into the deep system
- Duration: 14 to 45 days
- References
- Scovell in Eidt and Mills (2021) UpToDate, accessed 2/17/2022
IX. Course
- Most Superficial Thrombophlebitis resolves with symptomatic management
- Upper extremity Thrombophlebitis uncommonly progresses to DVT (except in cases of PICC Line Thrombosis)
X. Resources
- Czysz (2022) Superficial Thrombophlebitis, StatPearls, Treasure Island
XI. References
- DeLoughery and Orman in Majoewsky (2012) EM:Rap 12(12): 4-5
- Litin (2017) Cases from Anticoagulation Clinic, Mayo Clinical Reviews, Rochester, MN
- Kearon (2012) Chest 141:419S-94S [PubMed]