II. Epidemiology
- Deep Vein Thrombosis (DVT) represents 66% of Venous Thromboembolism (VTE)
- Pulmonary Embolism (PE) represents the remaining 33% of VTE
- Pulmonary Embolism accompanies proximal DVT in 40% of cases
- Deep Vein Thrombosis is identified in 70% of those with Pulmonary Embolism
- Venous Thromboembolism
III. Pathophysiology
- VTE is caused by at least one of three dysfunctions (Virchow's Triad)
- Hypercoagulability
- Blood Flow alterations
- Endothelial injury or dysfunction
IV. Risk Factors
- See Deep Vein Thrombosis Risk Factors (includes Recurrent Thromboembolism Risks)
- See Thrombophilia
- May Turner Syndrome
- Compressed right iliac common artery (RICA) results in ileofemoral DVT
- Arterial variants of RICA predispose to compression
- Resulting RICA pressure against lumbar bony Vertebrae resulting in bony spur formation
- Spurs and RICA compress iliac veins, resulting in DVT (esp. Left ileofemoral DVT)
- More common in women (RR 2)
- Responsible for 2 to 5% of DVTs (esp. females in their teens and twenties)
V. History
- Deep Vein Thrombosis Related
- Recent Surgery (esp. in the last 3 months, and esp. orthopedic surgery)
- Recent prolonged travel (esp. in the last 2 weeks, and esp. >10,000 km or 6200 miles)
- Prolonged sitting >3 to 4.5 hours at a time
- Hypercoagulable State or Thrombophilia (personal or Family History)
- Congestive Heart Failure
- General Immobility
- Malignancy
- Current or recent pregnancy
- Tobacco Abuse
- Hormonal therapy (esp. Oral Contraceptives)
- Pulmonary Embolism Related
- Other cause related history
VI. Exam
- See Localized Edema
- See Brief Musculoskeletal Exam
- Complete extremity neurovascular exam with comparision to opposite side
- Careful exam to differentiate causes of Localized Edema (and associated erythema and pain)
VII. Signs
- Unilateral extremity edema
- Bilateral DVT occurs in 7-20% of cases (even when only unilateral symptoms)
- Associated affected extremity findings (variable)
- Erythema
- Warmth
- Extremity Pain
- Clinical exam is unreliable for excluding DVT
- Homans' Sign (no predictive value)
- Homans' Sign: Relaxed foot abnormally plantar flexed
- Pseudo-Homans': Pain on passive dorsiflexion of foot
- Other unreliable signs
- Tenderness
- Distal extremity edema
- Palpable cord
- Homans' Sign (no predictive value)
- Significant DVT related extremity edema complications
- Phlegmasia Alba Dolens
- Pale white, severely edematous extremity (milk leg) with patent collateral veins
- Phlegmasia Cerulea Dolens
- Cyanotic or blue, severely edematous extremity (Copper leg) with obstructed collateral veins
- Phlegmasia Alba Dolens
VIII. Differential Diagnosis
- See Localized Extremity Swelling
- Extremity Trauma
- Cellulitis
- Peripheral Arterial Disease
- Baker's Cyst (Pseudo-thrombosis)
- Superficial Thrombophlebitis
- Fat Embolism
- Complicates 0.5 to 2% of long bone Fractures
- Classic triad presentation is Orthopedic Trauma with Petechiae, Dyspnea and Altered Mental Status
IX. Diagnosis
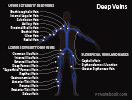
- Images
- Precautions
- See DVT in Pregnancy
- Exercise caution in pregnancy
- Pregnancy is higher risk of pelvic DVT (which is higher risk of PE and more difficult to detect)
- Step 1: Assess DVT Probability
- See Wells Clinical Prediction Rule for DVT
- If moderate to high probability, goto step 3
- Low probability Wells score does NOT exclude DVT (risk is still up to 5%)
- Step 2: Low Probability for DVT
- Obtain D-Dimer
- See D-Dimer for Discriminatory values (typically normal D-Dimer <=0.5 in age <50 years old)
- Negative D-Dimer: Excludes DVT in a low probability patient
- However, D-Dimer Test Sensitivity is 95%, and will miss 5% of DVTs
- Positive D-Dimer: Lower Extremity Doppler Ultrasound
- Negative Ultrasound
- Excludes DVT
- Positive Ultrasound
- Treat as DVT
- Negative Ultrasound
- Step 3: Moderate to high Probability for DVT
- Obtain Lower Extremity Doppler Ultrasound (Test Sensitivity approaches 95%)
- Negative compression Ultrasound: Obtain D-Dimer
- Negative D-Dimer
- Excludes DVT
- Positive D-Dimer
- Repeat compression Ultrasound in one week or obtain CTV (venography) for pelvic DVT
- Negative D-Dimer
- Positive compression Ultrasound
- Treat as DVT
- References
X. Associated Conditions
- See Thrombophilia
- Idiopathic DVT associated with undiagnosed malignancy
XI. Evaluation: Unprovoked Venous Thromboembolism
-
Thrombophilia
- See Thrombophilia for testing indications
- Consider directed screening in unprovoked VTE when diagnosis impacts management
- Malignancy
- Associated with a higher VTE recurrence rate (esp. brain, myeloproliferative, ovarian, lung and non-rectal GI cancer)
- Present in 20% of patients with VTE
- Relative Risk of malignancy diagnosis in 2 years: 3.0
- Prevalence of occult malignancy in unprovoked VTE: 3.9%
- Perform age and gender appropriate routine malignancy screening
- No other occult malignancy testing recommended (unless dictated by signs and symptoms)
- Atypical location (e.g. splenic or cerebral vein) may warrant additional testing
- Recurrence despite Anticoagulation, Family History and weight loss may also prompt evaluation
XII. Management: General
- See DVT in Pregnancy
- See Pulmonary Embolism Management
- Anticoagulation protocols are the same for DVT and PE
- Consider Thrombophilia work-up
- See Thrombophilia
- Reserve blood for tests prior to Anticoagulation
- Anticoagulation Protocol
- Disposition
- Local measures
- Early ambulation
- Replaces prior recommendations to minimize activity for first few days
- Elevate affected limb to reduce swelling
- Apply heat to affected limb
- Graded elastic Compression Stockings (20-30 mmHg)
- Early ambulation
-
Superficial Venous Thrombosis
Anticoagulation indications
- See Superficial Venous Thrombosis
- Proximal superficial clot (upper thigh) especially within 5 cm of deep system
- Clot >7 cm long in leg
- Lack of improvement after 1 week
- Hypercoagulable state
XIII. Management: Distal DVT (Calf-vein DVT)
- Option 1: Anticoagulation (standard strategy since 2001)
- Anticoagulation recommended for 6 to 12 weeks
- Initiate with LMWH and then to oral Warfarin (or other Anticoagulant - see above)
- Justification (based on risk of untreated calf DVT complications)
- Risk of propogation to proximal DVT is 5-20% (NNT 16)
- Recurs in 30% of untreated patients
- Post-Thrombotic Syndrome occurs in 20% if untreated
- Pinede (2001) Circulation 103:2453-60 [PubMed]
- Utter (2016) JAMA Surg 151(9): e161770 +PMID:27437827 [PubMed]
- Anticoagulation recommended for 6 to 12 weeks
- Option 2: 2015 Chest Guidelines recommend serial Ultrasound instead of Anticoagulation
- Assumes lower risk patient
- Asymptomatic
- No cancer history or other underlying Coagulopathy
- DVT not unprovoked and not recurrent
- Preferred strategy if Anticoagulation contraindicated or increased bleeding risk
- Safe even in symptomatic patients, with similar outcomes to Anticoagulation, but without the 4% bleeding risk
- Repeat Doppler Ultrasound twice weekly for 2 weeks
- Monitor for extension of distal DVT to proximal DVT
- Kearon (2016) Chest 149(2): 315-52 +PMID:26867832 [PubMed]
- Assumes lower risk patient
XIV. Management: Anticoagulation
XV. Management: Home Deep Vein Thrombosis Protocol
- Criteria for home management
- No massive Deep Vein Thrombosis
- No entire Leg Swelling, acrocyanosis or ischemia
- No DVT extension into iliofemoral vein or IVC
- No symptomatic Pulmonary Embolism
- Oxygen Saturation >95% on room air
- No significant bleeding risks on Anticoagulants
- Active bleeding or bleeding in last 4 weeks
- Recent surgery or Trauma
- Platelet Count <70, INR >1.4 or PTT >40 sec
- Metastatic disease involving liver or brain
- No significant comorbidities
- No severe liver or Kidney disease
- Impaired cognition or mobility
- Pain requiring ParenteralNarcotics
- References
- No massive Deep Vein Thrombosis
- Efficacy
- Safe and effective management of proximal DVT
- Spyropoulos (2002) Chest 122:108-14 [PubMed]
- Review Contraindications
- Use only in otherwise low risk patients
- See Low Molecular Weight Heparin for contraindication
-
Patient Education
- Demonstrate self-administered Subcutaneous Injections
- Review sterile technique
- Review risks of bleeding and infection
- Emphasize precautions against Trauma
- Consider home health referral
- Anticoagulation
XVI. Management: Intervention Radiology directed Thrombolysis (with benefit)
- Ileofemoral DVT (typically within last 14 days)
- High risk of comorbidity
- Post-Thrombotic Syndrome: >50%
- Venous Claudication at 5 years in nearly half of patients
- Efficacy data (some studies question longterm benefit)
- Normal vein after Catheter Thrombolysis: 45% (contrast with 0% after Heparin alone)
- Decreases risk of long term Venous Insufficiency, Post-Phlebitic Syndrome, stasis ulcers
- Best outcome if performed early (within 2 weeks)
- Poor efficacy if prior Deep Vein Thrombosis
- References
- High risk of comorbidity
- Other indications
- Massive proximal extremity DVT with severe symptoms or Limb Threatening Ischemia
XVII. Complications
-
Pulmonary Embolism (PE)
- PE is an increased risk in the first 2 weeks after DVT diagnosis and Anticoagulation start
- One third of DVT patients have an associated asymptomatic PE
-
Post-Thrombotic Syndrome (Postphlebitic Syndrome)
- Affects up to 50% of DVT patients, with chronic symptomatic Venous Insufficiency
- Reduced with below knee graded Compression Stockings
- Encourage 30 minute walk per day
-
Breakthrough Venous Thromboembolism
- See Prognosis below
- Occurs in 2 to 3% of VTE patients on Anticoagulation for 6 months
- Considered Breakthrough VTE if occurs at least 2 weeks after consistent Anticoagulation initiated
-
Phlegmasia (Milk Leg)
- Rare, high risk complications (mortality approaches 20 to 50%)
- Phlegmasia Alba Dolens
- Painful, white leg following ileo-femoral deep vein obstruction with patent superficial collateral
- Phegmasia Cerulea Dolens
- Painful, cyanotic, edematous leg following combined ileo-femoral deep AND superficial vein obstruction
- Venous Gangrene (capillary obstruction) results if not promptly managed
XVIII. Prognosis
- Overall mortality is increased in DVT patients
- Month 1: Mortality 3 to 6%
- Year 1 Mortality 13%
- Year 10 Mortality 42%
- Year 30: Mortality 68%
- Sogaard (2014) Circulation 130(10): 829-36 [PubMed]
- Naess (2007) J Thromb Haemost 5(4): 692-9 [PubMed]
- Recurrence when not on Anticoagulation
- See Thromboembolism Risk Factors
- Provoked VTE with transient risk factors: 3.3% recurrence rate in first year
- Unprovoked VTE: 10.3% recurrence rate in first year (30% in first 10 years)
- Proximal DVT has a 4 fold higher risk of recurrence than distal DVT
- Central Pulmonary Embolism has higher risk of recurrence than peripheral PE
- Elevated D-Dimer 3 weeks after stopping Anticoagulation is associated with higher risk of VTE recurrence
XIX. Prevention
- See DVT Prevention
- See DVT Prophylaxis
- See DVT Prevention in Travelers
XX. Resources
- CDC: Venous Thromboembolism
XXI. References
- Feied in Marx (2002) Rosen's Emergency Med, p. 1210-33
- Jean-Louis and Sethuraman (2023) Crit Dec Emerg Med 37(7): 4-11
- AbuRahma (2001) Ann Surg 233(6):752 [PubMed]
- Forster (2001) Chest 119(2):572-9 [PubMed]
- Hull (2000) Arch Intern Med 160:229-36 [PubMed]
- Hyers (2001) Chest 119:176S-93S [PubMed]
- Lensing (1999) Lancet 253:479-85 [PubMed]
- Merli (2001) Ann Intern Med 134:191-202 [PubMed]
- Mount (2022) Am Fam Physician 105(4): 377-85 [PubMed]
- Nasir (2025) Am Fam Physician 112(4): 424-34 [PubMed]
- Ramzi (2004) Am Fam Physician 69:2841-8 [PubMed]
- Wells (2001) Thromb Haemost 86(1):499-508 [PubMed]
- Wilbur (2012) Am Fam Physician 86(10):913-9 [PubMed]