II. Epidemiology
-
Incidence
- Malaria is the most common life threatening disease for travelers
- Mosquito population is expected to as much as double with global warming (0.4 C) by 2020
- Europe and North America infections are typically due to travel
- European, North American traveler cases: 30,000/year
- U.S. Cases reported to CDC per year: 1500 to 2000 (out of 18 million U.S. travelers to Malaria endemic areas)
- Malaria was endemic to North America, but was eradicated in the mid-twentieth century
- Worldwide Infections: 300 million per year (up to 500 million/year)
- Children under age 5 years are disproportionately affected (esp. in sub-saharan africa)
- Chloroquine-resistant P. Falciparum Malaria kills 500,000 young children/year in Africa alone
- Worldwide Mortality: 1-3 Million deaths per year
- Malaria (esp. P. falciparum) is among the top three infectious causes of death in the world
- Other high mortality infectious causes include HIV Infection and Tuberculosis)
- Children under age 5 years are disproportionately affected (esp. in sub-saharan africa)
- Timing
- Majority of Malaria outbreaks occur between May and December
- Highest risk is during and after the rainy season
- River beds and stagnant pools of water are most common breading grounds
- Regions
- Endemic to tropical and subtropical world around the equator (106 countries as of 2010)
- Highest Risk
- Sub-Saharan Africa
- Papua New Guinea
- Solomon Islands
- Vanuatu
- Intermediate Risk
- Haiti
- Indian subcontinent
- Southeast Asia
- Low Risk
- Latin America
III. Pathophysiology
- See Vector-Borne Infection
- Transmitted by bite of female anopheline (or anopheles) Mosquito
- Usually bites between dusk and dawn
- Injects malaria Protozoa from Salivary Glands
- Other modes of human transmission (e.g. Blood Transfusion, congenital transmission) are rare
- Species of Malaria
- Plasmodium Falciparum (most common and most life threatening)
- Fulminant Malaria associated with high Parasitemia and intravascular congestion
- Incubation Period: Typically 12-14 days (ranges from 7 to 30 days)
- Most severe of disease with multiorgan involvement (esp. brain, liver)
- Responsible for most Malaria deaths
- Irregular fever cycles (every 36 to 48 hours), or with Continuous Fever and symptoms
- Chloroquine resistance (except in central america)
- Sickle Cell Trait is partially protective against P. falciparum infection
- Sickle Cell Trait impedes Malaria RBC infection and survival within RBCs
- Plasmodium Vivax
- Incubation Period: Months to years
- Fever recurs every 3 days (Tertian Fever at 48 hour intervals) as with P. ovale
- May cause latent phase (hypnozoites), dormant within the liver for months to years
- P. vivax requires red cell surface Antigens Duffy A and B for binding
- Red cell Antigens Duffy A and B are absent in >60% of black patients (88-100% in West Africa)
- Absent Duffy A and B is protective against Plasmodium Vivax
- Plasmodium Ovale
- Incubation Period: Months to years
- Fever recurs every 3 days (Tertian Fever at 48 hour intervals) as with P. vivax
- May cause latent phase (hypnozoites), dormant within the liver for months to years
- Plasmodium Malariae (Quartan Malaria)
- Fever recurs every 4 days (Quartan Fever at 72 hour intervals)
- Plasmodium knowlesi
- Emerging pathogen in those exposed to macque monkeys
- Similar in appearance to p. Malariae
- As with Plasmodium Falciparum, may cause severe disease
- Plasmodium Falciparum (most common and most life threatening)
- Life cycle of Malaria
- Injected from Mosquito as sporozoite
- Sporozoites are thin, spindle shaped, motile forms of Malaria
- Sporozoites traverse the human bloodstream to the liver
- Sporozoites invade hepatocytes in human liver (Pre-erythrocytic cycle)
- Sporozoites undergo asexual division within hepatocytes
- Sporozoites may lie dormant in liver (hypnozoites)
- Occurs with Plasmodium Vivax and Plasmodium Ovale
- Symptoms recur when reactivates in months to years
- Merozoites develop from Sporozoites after weeks to months of development within hepatocytes (liver cells)
- Thin spindle shaped sporozoite transitions to a round form (trophozoite) within infected liver cells
- Trophozoite nucleus divides into thousands of nucleii, forming a Schizont within the liver cell
- Schizont nucleii each form cytoplasmic membranes creating small intracellular bodies (Merozoites)
- Engorged liver cells rupture, releasing merozoites into the bloodstream
- Merozoites invade erythrocytes and circulate freely
- P. Malariae may remain in Red Blood Cells without lysis, latent for months to years
- Typically results in Red Blood Cell lysis within 48-72 hours of erythrocyte invasion
- In severe cases (esp. P. falciparum), up to 30% of Red Blood Cells may be infected
- Merozoites form round trophozoites within the infected red cell
- Trophozoite appears as a ring with nuclear material clustered in one portion (diamond on a ring)
- Multinucleated schizont forms from cell division of the Trophozoite (similar to hepatic cell process)
- New merozoites form as each nucleus is surrounded by a cytoplasmic membrane
- Hemolysis (Red Blood Cell lysis) with schizont expansion
- Non-lysed, but infected RBCs also have increased adhesion to other RBCs and vascular endothelium
- Results in both vascular Occlusion as well as Hemorrhages
- May result in end organ injury (esp. P. falciparum), including brain, Kidney and lung
- Hemolysis is associated with fever spikes (and overall immune/inflammatory response)
- Fever spikes typically occur randomly, but may occur with RBC lysis in a pattern
- May cause Tertian Fever (recurring every third day as with P. ovale and vivax)
- May cause Quartan Fever (recurring every fourth day as with P. Malariae)
- Some circulating merozoites differentiate into male and female Gametocytes
- Gametocytes are the sexual form of plasmodium (sexually dividing within the Mosquito)
- Contrast with asexual division in the human liver
- Male and female Gametocytes circulate in the human blood stream
- Mosquito ingests both male and female gametocytes from infected host
- Oocysts develop within the Mosquito over a 10-21 day course into sporozoites
- Resulting sporozoites are motile, thin spindle-shaped Protozoa
- Sporozoites spread throughout the Mosquito, including the mosquito Salivary Glands
- Mosquito infects next human host with bite, transmitting motile sporozoites via its Saliva
- Gametocytes are the sexual form of plasmodium (sexually dividing within the Mosquito)
- Injected from Mosquito as sporozoite
IV. Precautions
- Fever in a returning traveler from Malaria endemic area is Malaria until proven otherwise
- Up to 50% of Malaria cases are misdiagnosed on the first visit
- Initial presentations are often mild and non-specific (fever, chills, malaise, myalgia, Headache)
- Malaria (esp. P falciparum) requires emergent evaluation
- Clinical decompensation or death may occur within 24 to 36 hours in a Malaria naive patient
V. Symptoms
- Timing
- Presentation within the first month of return from travel to endemic region
- Plasmodium Falciparum Incubation Period is typically 12 to 14 days (range 7 to 30 days)
- See Fever in the Returning Traveler for timing of other illnesses in the differential
- Delayed presentation beyond 2 months may occur with the use of chemoprophylaxis
- Plasmodiun ovale and Plasmodium Vivax may have delayed presentations, months later
- Presentation within the first month of return from travel to endemic region
- Initial prodrome
- Headache
- Malaise
- Next
- Fever (>50% of patients)
- Shaking chills
- Drenching Night Sweats
- Next
- Drowsiness
- Lethargy
- Fatigue
- Other symptoms
- Myalgias
- More severe in Dengue Fever
- Muscle tenderness
- More severe in Leptospirosis and Typhus
- Arthralgias
- Back pain
- Gastrointestinal Symptoms (may be isolated presentation in children)
- Myalgias
VI. Signs
- Episodic fever for 1-8 hours
- May be persistent in P. falciparum
-
Fever recurs
- Plasmodium Vivax: 48 hour intervals (Tertian Fever)
- Plasmodium Malariae: 72 hour intervals (Quartan Fever)
- Plasmodium Falciparum: Variable
- Gastrointestinal findings (in <35-40% of cases)
- Increased splenic and hepatic activity results from Hemolysis
- Tender Splenomegaly (risk of Splenic Rupture)
- Hepatomegaly
- Severe Falciparum Malaria
- Hypotension and shock
- Multisystem failure
- Pulmonary Edema
- Acute Respiratory Distress Syndrome
- Renal Failure (1% of cases)
- Jaundice and liver failure (associated with poor prognosis)
- Cerebral Malaria
- Mortality approaches 15-20% in young children (<esp. age <5 years) even with treatment
- Altered Mental Status to unresponsive
- Seizures
- Meningism (uncommon but carries 23% mortality)
VII. Differential Diagnosis
- See Fever in the Returning Traveler
- See Vector-Borne Infection
- Arboviruses are also Vector-Borne Infections (Aedes aegypti Mosquito-Borne Disease is common vector)
- Rash is uncommon in Malaria (aside from Petechiae in severe Falciparum Malaria with DIC) and suggests other diagnosis
- Other Bacterial Infections
- Other Viral Infections
- Other Parasitic Infections
VIII. Labs
-
Blood Glucose
- Hypoglycemia may occur (esp. children)
-
Complete Blood Count (CBC) with differential
- Especially consider Malaria with Leukopenia and Left Shift, Thrombocytopenia
- Hemoglobin or Hematocrit consistent with Anemia (29%)
- Leukopenia with White Blood Cell Count <5000/mm3 (26%)
- Thrombocytopenia (45%)
- Bandemia (85%)
-
Urinalysis
- Urobilinogen positive
- Hemoglobinuria (rare, may occur with Plasmodium Falciparum)
-
Cerebrospinal Fluid Examination
- Indicated in Altered Mental Status and fever
- Exclude Meningitis and Encephalitis (esp. if Malaria diagnosis is unclear)
- Malaria CSF is typically normal (aside from mild CSF Pleocytosis, mild increased CSF Protein)
IX. Diagnosis
-
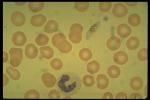
Peripheral Blood Smear
- Gold standard for diagnosis
-
Peripheral Smear is performed under oil-immersion, 1000x magnification
- Infected Red Blood Cells demonstrate intracellular trophozoites and schizonts
- Gametocytes may also be visualized in the peripheral blood external to RBCs
- Stains
- Giemsa stain (reference standard stain for Malaria evaluation with thick and thin smears)
- Thin blood smear (first-line Malaria evaluation)
- Giemsa stain of blood fixed with Alcohol to prevent Red Blood Cell lysis
- Thin stain can identify Malaria species and quantify Parasitemia
- High Test Sensitivity
- Thick blood smear (perform if thin blood smear negative)
- Giemsa stain of blood allowed to dry on slide (allowing cell lysis)
- Thick stain evaluates for malaria Parasites in general
- Thin blood smear (first-line Malaria evaluation)
- Wright stain (standard stain for most Complete Blood Count associated manual differentials)
- Test Sensitivity approaches that of Giemsa stain
- Giemsa stain (reference standard stain for Malaria evaluation with thick and thin smears)
- Protocol
- Stat blood smear with direct communication with reading pathologist (alert for Malaria concern)
- Examine new smear every 12-24 hours for 2-3 days (low Parasitemia may require additional smears)
- Sample is best obtained when patient is febrile
- Image
- Rapid blood dipstick testing (when smear not available)
- Tests
- Binax-NOW (only detect P. falciparum and P. vivax; only FDA approved test in U.S.)
- HRP-2 detection (only detects P. falciparum)
- LDH detection (detects all 4 Malaria types)
- Benefits
- Good Test Sensitivity and Negative Predictive Value, yet easy to perform and does not require lab facility
- Results available within 5 to 20 minutes
- Precautions
- All rapid tests should be followed by blood smears
- Positive tests do not quantitate Parasitemia
- Negative rapid tests should be confirmed with blood smears
- Decreased Test Sensitivity with low levels of Parasitemia
- Examples: Patients who took chemoprophylaxis, or prior exposure
- All rapid tests should be followed by blood smears
- Tests
- Malaria PCR
- Detects low levels of parsites in blood (<5 Parasites/ul)
- Distinguishes between plasmodium species
- May be used to monitor response to treatment at 5-8 days (however False Positives may occur)
X. Management: Falciparum or Knowlesi Malaria or Severe Case and Unknown Species
- See CDC emergency contact information as below for Malaria management guidance
- Precautions
- Substandard and counterfeit antimalarial use is widespread in resource limited and low income countries
- G6PD Deficiency
- Avoid Chloroquine, Primaquine, Quinine (due to Hemolysis risk)
- Anti-Malarials Considered safe in Pregnancy
- Chloroquine
- Hydroxychloroquine
- Quinine or Quinidine
- Clindamycin
- Mefloquin
- Sulfadoxine Pyrimethamine (second and third trimesters only)
- Artemisinin Combination Therapy (ACT) safe in second and third trimester
- Artemether/Lumefantrine (Coartem) may be used in first trimester if no other reasonable option
- Hospital Admission Criteria
- Admit P. Falciparum Malaria and P. Knowlesi cases to hospital (high mortality in first 48 hours)
- Also admit all undiferentiated cases where species of Malaria cannot be discerned
- High Risk Cohorts
- Immunocompromised
- Malaria naive patients (no prior Malaria infections)
- Children
- Pregnancy
- Severe case criteria (any of the following)
- Glasgow Coma Scale (GCS) <11 or Coma
- Seizures
- Severe Anemia (Hemoglobin <7 g/dl in adults, <5 g/dl in children age <12 years)
- Acute Kidney Injury
- Hypoglycemia
- Acute Respiratory Distress Syndrome
- Shock
- Disseminated Intravascular Coagulation
- Acidosis
- Liver Dysfunction
- Parasite Density >5%
- Admit P. Falciparum Malaria and P. Knowlesi cases to hospital (high mortality in first 48 hours)
-
Artemisinin Combination Therapy (ACT) Antiparasitic Agents (2 agents)
- Regimens based on severity (see above for severe case criteria)
- General Protocol
- Agent 1: Artemisinin (or dihydroartemisinin, Artemether, or Artesunate) - first-line agent
- See Artesunate (preferred in U.S.)
- Artemisinin is contraindicated in first trimester of pregnancy
- Use oral formulation in non-severe cases, and intravenous formulation in severe cases
- Agent 2: Lumefantrine (see below), Chloroquine, Sulfadoxine-Pyrimethamine (Fansidar) or Mefloquine
- Treat for 3 days (6 days if travel to areas with high Malaria resistance)
- Agent 1: Artemisinin (or dihydroartemisinin, Artemether, or Artesunate) - first-line agent
- Non-Severe Cases: Artemether/Lumefantrine (Coartem)
- Each tablet contains 20 mg Artemether (an Artemisinin) and 120 mg Lumefantrine
- Tablets may be crushed and mixed with 10 ml water if unable to swallow tablets (e.g. children)
- Tablets are best absorbed with high fat foods
- Repeat dose if Vomiting occurs within 2 hours of dose
- Each dose based on weight
- Children 5 kg to 15 kg: 1 tablet per dose
- Children 15 kg to 25 kg: 2 tablets per dose
- Children 25 kg to 35 kg: 3 tablets per dose
- Children >35 kg and Adults: 4 tablets per dose
- Dosing (3 day course, with doses per weight as above)
- Give one dose every 8 hours for 2 doses on day 1, then one dose every 12 hours on days 2 and 3
- Each tablet contains 20 mg Artemether (an Artemisinin) and 120 mg Lumefantrine
- Severe Cases: Intravenous Artemisinin (Artesunate is preferred)
- Indicated in severe cases (see criteria above), including Parasite load >5%
- Start immediately at the time of diagnosis
- Artesunate 2.4 mg/kg at start, 12 and 24 hours, then daily until Parasitemia <1% (up to 7 days)
- Obtain blood smear Parasite stains for density every 12 hours
- Other agents when Artemisinin Combination Therapy (ACT) is unavailable
- Chloroquine sensitive regions
- Chloroquine
- Adults
- Load: 1000 mg salt (600 mg base) orally at start
- Maintenance: 500 mg salt (300 mg base) orally at 6 hours, 24 hours and 48 hours after initial dose
- Child
- Load: 16.7 mg/kg salt (10 mg/kg base) orally at start
- Maintenance: 8.3 mg/kg salt (5 mg/kg base) orally at 6 hours, 24 hours and 48 hours after initial dose
- Adults
- Hydroxychloroquine (Plaquenil)
- Adult: 800 mg salt (620 mg base) to start, then 400 mg salt (310 mg base) at 6, 24 and 48 hours after initial dose
- Child: 12.9 mg/kg salt (10 mg/kg base) to start, then 6.5 mg/kg salt (5 mg/kg mg base) at 6, 24 and 48 hours after initial dose
- Chloroquine
- Chloroquine resistant regions
- Atovaquone/Proguanil (Malarone)
- See Atovaquone for dosing
- Quinine-based protocols (2 agents)
- General
- Avoid in severe disease
- Use 7 day course if acquired in Southeast Asia
- Quinine 10 mg/kg up to 648 mg salt (8.3 mg/kg up to 542 mg base) three times daily orally for 3 to 7 days AND
- Second Agent
- Doxycycline 2.2 mg/kg up to 100 mg orally twice daily for 7 days (or Tetracycline) OR
- Clindamycin (if Tetracyclines contraindicated) 20 mg/kg orally for 3 to 7 days
- General
- Mefloquine (other options are preferred)
- Adult: 750 mg salt (684 mg base) for first dose, then second dose of 500 mg salt (456 mg base) in 6 to 12 hours
- Child: 15 mg/kg salt (13.7 mg/kg base) for first dose, then second dose of 10 mg/kg salt (9.1 mg/kg base) in 6 to 12 hours
- Atovaquone/Proguanil (Malarone)
- Chloroquine sensitive regions
- Plasmodium Malariae and Plasmodium knowlesi
- Artemisinin Combination Therapy (ACT) is recommended despite lack of Chloroquine resistance (see protocol below)
- Admit all Plasmodium knowlesi cases (high risk for severe disease)
- Following Initial Treatment: Plasmodium Ovale or Plasmodium Vivax (risk of relapsing infection)
- Risk of dormant Malaria (due to hypnozoites) and relapsing infection
- Follow initial course with following therapies to prevent relapsing infection
- Mothers infected with P. vivax or P. ovale during pregnancy
- Test infants for G6PD Deficiency after delivery
- Mothers should Breast feed and take either Primaquine (No G6PD Deficiency) or Chloroquine (G6PD deficient)
- No G6PD Deficiency
- Primaquine
- Adult: 52.6 mg salt (30 mg base) orally daily for 14 days after initial course
- Child: 0.8 mg/kg salt (0.5 mg/kg base up to 30 mg/day) orally daily for 14 days after initial course
- Decrease dose if Tinnitus or hyperexcitability occur
- Tafenoquine
- Adult (>age 16 years): 300 mg orally once after first or second day following Chloroquine course
- Contraindicated age <16 years or Psychotic Disorder
- Use only if Chloroquine or Hydroxychloroquine were used to treat initial infection
- Primaquine
- G6PD Deficiency
- Continue Chloroquine prophylaxis 500 mg salt (300 mg base) dosed weekly for one year OR
- Primaquine may be considered if G6PD is mild or intermediate
- Consult infectious disease
- Risk of dormant Malaria (due to hypnozoites) and relapsing infection
- Specific complication management
- Shock
- Intravenous hydration (including fluid boluses)
- Obtain Blood Cultures and add Third Generation Cephalosporin to regimen
- Cerebral Malaria (18% of cases)
- Seizures
- Supportive care including intubation may be needed
- Meningism (see above, uncommon but carries 23% mortality)
- Bleeding
- Coagulopathy reversal
- Blood Transfusion
- Shock
- Other non-specific management
- Intravenous Fluids
- Antipyretics
- Antiemetics
- Follow-up
- Evaluate for Hemolytic Anemia at 30 days after treatment of severe cases
XI. Prevention
- Malaria specific prevention
- Malaria Chemoprophylaxis is critical and not taken adequately in as many as 75% of U.S. travelers
- Malaria Vaccine
- WHO has recommended use for Malaria falciparum prevention in children
- Vaccination initiated in 2021 in Ghana, Malawi and Kenya (>1 million doses administered as of 2022)
- Alonso (2022) N Engl J Med 386(11): 1005-7 [PubMed]
- Prevent anopheles Mosquito Bites
- See Prevention of Vector-borne Infection
- Stay in air conditioned or well screened rooms
- Reduce nighttime outdoor activity (Dusk until dawn)
- Apply an effective Insect Repellent
- DEET 20 to 30% to skin every 3-4 hours or
- Picaridin 20% or
- p-Menthane-3,8-diol (PMD, Menthoglycol)
- Spray clothing and bed nets with Permethrin
- Wear long sleeve shirt and pants
- Use Insecticide aerosols at dusk in living areas
- Use a strong fan at bedside
- Use Mosquito bed netting even in hotel rooms
- Mosquito net pre-treated with Permethrin
- Reapply Permethrin every 6 months
XII. Complications
- Encephalopathy (Cerebral Malaria)
- Seizures and coma
- High mortality (esp. children)
- Hypoglycemia
- Acute Renal Failure
- Hepatic Dysfunction
- Pulmonary Edema
- Disseminated Intravascular Coagulation
- Hemolytic Anemia
- Shock
XIII. Prognosis
- Plasmodium Falciparum Mortality: 4% (20% in severe cases)
- More severe cases in children and pregnant women
XIV. Resources
- See Travel Resources
- CDC Malaria hotline (health care professionals)
- https://www.cdc.gov/parasites/contact.html
- Phone: 770-488-7788 (daytime, Monday to Friday, 9 am to 5 pm Eastern Standard Time)
- Phone: 855-856-4713 (daytime, toll free)
- Phone: 770-488-7100 (after hours, emergency operations center, ask to speak with DPDM expert)
- CDC Malaria Information
- Malaria Foundation International
XV. References
- Gladwin, Trattler and Mahan (2014) Clinical Microbiology, Medmaster, Fl, p. 343-6
- Anderson (2014) Crit Dec Emerg Med 28(7): 11-9
- Black, Martin, DeVos (2018) Crit Dec Emerg Med 32(8): 3-12
- Mason and Marsh in Herbert (2019) EM:Rap 19(5):12-3
- Nordurft-Froman and DeVos (2022) Crit Dec Emerg Med 36(4): 4-15
- Baird (1999) Med Clin North Am 83(4):923-44 [PubMed]
- Croft (2000) BMJ 321(7254):154-60 [PubMed]
- Feder (2013) Am Fam Physician 88(8): 524-30 [PubMed]
- Johnson (2012) Am Fam Physician 85(10): 973-7 [PubMed]
- Lo Re (2003) Am Fam Physician 68(3):509-16 [PubMed]
- Shahbodaghi (2022) Am Fam Physician 106(3): 270-8 [PubMed]