II. Epidemiology
- Incidence: 17-35% in Nursing Home residents
- Prevalence: 3 Million treated patients in U.S. per year
- Estimated to cost $11 to 26 Billion per year in U.S.
III. Pathophysiology
- External localized pressure exceeds capillary Blood Flow to affected region
- Results ischemia and injury to local tissue, skin and mucosa
- Shearing forces add to the degree of Pressure Injury
IV. Risk Factors
- Key risk factors
- Non-Ambulatory Patients or limited mobility
- Decreased perfusion
- Local tissue edema
- Pre-existing Stage 1 Pressure Sore
- Excessive moisture (e.g. bowel or bladder Incontinence, wound drainage, excessive sweating)
- Other risk factors
- Underweight, malnourished or Cachexia
- Cognitive Impairment or Dementia
- Incontinence (and other causes of excessive moisture)
- Advanced age
- Device-induced pressure (e.g. Nasogastric Tube, Nasal Cannula, casts or splints)
- Higher risk medical conditions
- Diabetes Mellitus
- Congestive Heart Failure
- Peripheral Vascular Disease
- Neurologic disorders (e.g. Dementia, Multiple Sclerosis, Parkinsonism, Spinal Injury, Stroke)
V. Signs: Distribution
VI. Exam: Pressure Injury Characterization
- See Comprehensive Skin Integrity Assessment
- Basic description
- Include images and diagrams in EHR
- Location
- Size (Length x Width x Depth)
- Timing (onset and progression)
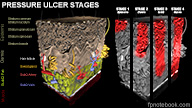
- Stage (Types 1-4)
- See Decubitus Ulcer Grade
- Staging precautions
- Accurate grading requires Debridement of necrosis first
- Use other grading schemes for staging of Diabetic Foot Ulcers and Venous Stasis Ulcers
- Macerated skin (moisture induced wounds) are not staged
- Stage 1: Nonblanchable erythema of intact skin (pink skin, not purple)
- Stage 2: Superficial or partial thickness skin loss (no slough or eschar)
- Stage 3: Full thickness skin loss with subcutaneous damage (crater to fascia)
- Stage 4: Full thickness skin loss with extensive deep damage to Muscle, bone, tendon
- Additional findings
- Sinus tracts, skin undermining or tunneling
- Exudate or sloughing
- Necrotic tissue
- Granulation tissue
- Wound discharge
- Wound odor
- Signs of Wound Infection or Cellulitis
- Skin base quality and surrounding skin integrity
- Wound bed color
-
Wound Healing Assessment Tools
- Pressure Ulcer Scale for Healing
- DESIGN-R (depth, exudates, size, inflammation, granulation, necrosis, rating)
- Bates-Jensen Wound Assessment Tool
- Images
VII. Labs
-
Wound culture
- Typically not indicated except to identify MRSA
- Levine Technique is preferred
- Rotate culture swab over a 1 cm patch of wound
- Apply enough pressure for fluid to collect in wound site for 5 seconds
- Reddy (2012) JAMA 307(6): 605-11 [PubMed]
VIII. Differential Diagnosis
- See Leg Ulcer Causes
- Stasis ulcer
- Ischemic ulcer (Peripheral Vascular Disease)
- Vasculitic ulcer
IX. Management: General Approach
- See TIME Principle of Chronic Wound Care
- Monitoring
- Weekly clinical assessment
- Daily observation by Caregiver
- Key point: Minimize moisture, friction and sheering
- Control moisture and keep skin clean and dry, and with barrier creams applied
- Without this, no Pressure Sore will heal
- Consider modified beds or bed overlays (see Pressure Sore Positioning)
- Protect normal skin at wound edges
- Use Wound Dressings or Emollients to protect skin from moisture and irritation
- Patient positioning to take pressure off wound
- See Pressure Sore Positioning
- See Decubitus Ulcer Prevention
- Remove all pressure at the ulcer site
- Frequent repositioning (every 2 hours)
- Do not drag patient
-
Wound cleaning and Debridement
- See Decubitus Ulcer Cleansing
- See Decubitus Ulcer Debridement
- Manage the microclimate
- Use a pH neutral skin cleanser
- Use barrier wipes and creams
- Avoid removing a dry, non-inflamed, non-fluctuant intact eschar at heel
- Provides intact barrier to further injury
- Nutrition
- See Nutrition in Wound Healing
- Ensure adequate hydration per day
- Correct Malnutrition and specific deficiencies
- Supplement Protein 1.25 to 1.5 g/kg bodyweight
- Supplement calories 30 to 35 kcal/kg bodyweight
- Consider Vitamin Supplementation (e.g. Zinc, Arginine, Vitamin C)
- Control sources of pain
- Cover wounds
- Adjust support surfaces
- Reposition patient frequently
- Provide analgesia with dressing changes and Debridement
- Control moisture
- Contributes to maceration and skin breakdown
- Airflow surface may help keep area dry
- Do not use Incontinence briefs (impedes airflow)
- Be alert for signs of infection
- Delayed Wound Healing
- Wound dehiscence
- Local tissue necrosis
- Increased exudate
- Increased local warmth
- Cellulitis
- Osteomyelitis suspected (exposed bone or Probe-to-Bone Test positive)
- Systemic signs (fever, Altered Mental Status, increased pain)
- Other measures
- Smoking Cessation
- Caregiver Support and education
- Psychosocial support for patient and Caregivers
X. Management: Wound Dressing
- See Wound Dressing for complete list and selection criteria
- Precautions
- Cleanse wounds before each dressing change
- Debride wounds with overlying slough or biofilm
- See Decubitus Ulcer Debridement
- Avoid Debridement of slough on the heels or ischemic limbs
- Dressings should promote moist Wound Healing (without being wet)
- Avoid Wet-to-Dry Dressings
- May slow healing and results in pain on removal
- Wet-to-Moist Dressing however may be used (see below)
- Protect normal skin on wound edges to prevent progression
- See above
-
Decubitus Ulcer Grade 1 (red but intact skin)
- Apply barrier protection
- No dressing is typically needed
- Consider Transparent Film Dressing (e.g. Tegaderm)
-
Decubitus Ulcer Stage 2 (superficial or partial thickness skin loss)
- Light Exudate
- Hydrogel Dressing (provide moisture to dry wounds)
- Heavy Exudate (absorbent dressing)
- Hydrocolloid Dressing (e.g. Duoderm CGF) with or without absorbent paste or powder
- Light Exudate
-
Decubitus Ulcer Stage 3 to 4
- Shallow - Dry wounds
- Thin Hydrocolloid Dressing (e.g. Tegaderm Thin, Primacol Thin, Restore Extra Thin)
- Hydrogels (provide moisture to dry wounds)
- Transparent Film Dressing (e.g. Tegaderm)
- Wet-to-Moist Dressing
- Cover with nonadherent gauze wrap
- Shallow - Wet wounds
- Hydrocolloid Dressing (e.g. Duoderm CGF) with or without absorbent paste or powder
- Cover with nonadherent gauze wrap
- Shallow - Very Wet wounds
- Foam Dressing (e.g. Allevyn) - preferred
- Alginate Dressing
- Cover with nonadherent gauze wrap
- Deep - Dry wounds
- Fill wound with damp gauze or Hydrogel Dressing
- Cover with Hydrocolloid Dressing
- Cover with Transparent Film Dressing (e.g. Tegaderm) or nonadherent gauze wrap
- Deep - Wet wounds
- Foam Dressing (e.g. Allevyn)
- Consider filling with Alginate Dressing
- Cover with Transparent Film Dressing (e.g. Tegaderm)
- Shallow - Dry wounds
- Infected Wounds
- Superficially Infected Wounds
- Topical antimicrobials or Antimicrobial Dressing
- Spreading Wound Infection (e.g. Cellulitis)
- Perform Wound Debridement and send material for culture and sensitivity
- Start systemic Antibiotics
- Consider underlying Osteomyelitis
- Superficially Infected Wounds
XI. Management: Adjunctive Therapy for Grade 3 to 4 Ulcers
- Electrotherapy (Electrical stimulation)
- Direct electric, pulse current via electrodes applied to wound bed for 1 hour daily
- Indicated in Grade 3-4 Pressure Ulcers refractory to other care
- Contraindicated in cancer and Osteomyelitis
- Kawasaki (2014) Wound Repair Regen 22(2): 161-73 [PubMed]
- Ultrasound
- Vacuum-Assisted Closure (negative pressure)
- Collagen matrix dressing (bovine, porcine or avian)
- Insufficient evidence to support use of other adjuncts
- Topical and systemic agents
- Hyperbaric treatment
- Infared or ultraviolet light exposure
XII. Course
- Anticipate Wound Healing over 2 to 4 weeks
XIII. Complications
-
Osteomyelitis
- Suspect if non-healing ulcer after 2 to 4 weeks
- Presume Osteomyelitis when bone is exposed within wound site
- Start with plain film, but typically requires bone scan or MRI
- Consult infectious disease
-
Cellulitis (Bacterial superinfection) or Sepsis
- Stage 2 and greater Pressure Ulcers are colonized with Bacteria
- Adequate cleansing and Debridement prevents infection
- Size and depth of ulcer does not distinguish need for Antibiotics
- Risk factors for infection
- Foreign bodies within ulcer
- Large or necrotic ulcers
- Repeatedly contaminated sites (e.g. stool at Sacrum)
- Diabetes Mellitus or Immunosuppression
- Diminished perfusion
- Findings suggestive of infection
- Increasing pain is a a key indicator of Wound Infection
- Fever
- Leukocytosis
- Increased purulent or foul discharge
- New necrotic tissue
- Surrounding erythema
- Irregular or friable granulation tissue
- Wound culture is typically not indicated
- Consider if determining presence of MRSA
- See Levine culture technique described above
XIV. Prevention
XVI. References
- (2015) Presc Lett 22(5): 29
- Vertanen (2017) Wound Care Update, Park Nicollet Conference, St Louis Park, MN (attended 9/15/2017)
- Habif (1996) Clinical Derm, Mosby, p. 810-13
- PUGP (1994) Pressure Ulcer Treatment, AHCPR 95-0653
- PUGP (1995) Am Fam Physician 51(5):1207-22
- Krasner (1995) Prevention Management Pressure Ulcers
- Lewis (1996) Med-Surg Nursing, Mosby, p. 199-200
- Lueckenotte (1996) Gerontologic Nurs., Mosby, p. 800-7
- Way (1991) Current Surgical, Lange, p.95-108
- Bello (2000) JAMA 283(6): 716-8 [PubMed]
- Bowers (2020) Am Fam Physician 101(3):159-66 [PubMed]
- Degreef (1998) Dermatol Clin 16(2): 365-75 [PubMed]
- Findlay (1996) Am Fam Physician 54(5): 1519-28 [PubMed]
- Knapp (1999) Pediatr Clin North Am 46(6):1201-13 [PubMed]
- Raetz (2015) Am Fam Physician 92(10): 888-94 [PubMed]
- Stotts (1997) Clin Geriatr Med 13(3): 565-73 [PubMed]
- Qaseem (2015) Ann Intern Med 162:359-9 [PubMed]
- Visconti (2023) Am Fam Physician 108(2): 166-74 [PubMed]