II. Indications
- Patients at high risk of Pressure Injury (e.g. Decubitus Ulcer)
- See Pressure Injury
III. Timing
- Perform baseline exam on inpatient or Skilled Nursing Facility Admission
- Perform at periodic intervals, adjusted for acuity of illness and clinical status changes
IV. Exam: General
- Perform full skin exam, uncovering all surfaces for examination
- Focus on bony prominence regions and areas of medical device contact (see Decubitus Ulcer)
- Evaluate skin integrity
- Erythema (blanchable or nonblanchable?)
- Skin firmness
- Moisture
- Pain or tenderness
- Temperature variation
V. Exam: Pressure Injury Characterization
- See Pressure Injury
- See Comprehensive Skin Integrity Assessment
- Document each region of Pressure Injury (with images taken for the EHR)
- Basic description
- Include images and diagrams in EHR
- Location
- Size (Length x Width x Depth)
- Timing (onset and progression)
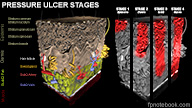
- Stage (Types 1-4)
- See Decubitus Ulcer Grade
- Staging precautions
- Accurate grading requires Debridement of necrosis first
- Use other grading schemes for staging of Diabetic Foot Ulcers and Venous Stasis Ulcers
- Macerated skin (moisture induced wounds) are not staged
- Stage 1: Nonblanchable erythema of intact skin (pink skin, not purple)
- Stage 2: Superficial or partial thickness skin loss (no slough or eschar)
- Stage 3: Full thickness skin loss with subcutaneous damage (crater to fascia)
- Stage 4: Full thickness skin loss with extensive deep damage to Muscle, bone, tendon
- Additional findings
- Sinus tracts, skin undermining or tunneling
- Exudate or sloughing
- Necrotic tissue
- Granulation tissue
- Wound discharge
- Wound odor
- Signs of Wound Infection or Cellulitis
- Skin base quality and surrounding skin integrity
- Wound bed color
- Images
VI. Resources: Wound Healing Assessment Tools
- Pressure Ulcer Scale for Healing
- DESIGN-R (depth, exudates, size, inflammation, granulation, necrosis, rating)
- Bates-Jensen Wound Assessment Tool