II. Indications
- Asthma Diagnosis and Asthma Management (all cases from age 5 years old and older)
-
COPD Diagnosis and COPD Management (all cases)
- Acute decompensation risk increases significantly at FVC <1-1.5 L (esp. with Muscle Weakness, chest wall deformity)
- Vesbo (2013) Am J Respir Crit Care Med 187(4): 347-65 [PubMed]
- Restrictive Lung Disease
- Dyspnea Evaluation
- Neuromuscular disorders (e.g. Myasthenia Gravis, Guillain Barre Syndrome)
III. Precautions
- Pulmonary Function Tests are primarily indicated for diagnosis of stable patients (not Acute Respiratory Failure)
-
Vital Capacity and Forced expiratory flow may be used in acute presentations who are alert (esp. to compare to baseline PFTs)
- FEV1 <1-1.5 L significantly increases the risk of caute Respiratory Failure
V. Criteria: Adequate test (Minimum of 3 tests)
- Full inhalation
- Maximal exhalation
- No cough or glottic closure (or other artifacts in the flow-volume loop)
- Flow-volume loop should reach a baseline plateau at the end of expiration (right side of the loop) prior to inspiratory loop
- Adequate test duration (exhale for 6 or more seconds)
- No mouth-piece leak
- Variation between two best effort tests are within 5%
- Difference between 2 largest FVC <0.2 L
- Difference between 2 largest FEV1 <0.2 L
VI. Protocol: Patient Preparation
- Stop Bronchodilators before test (Corticosteroids may be continued)
- Stop Short-acting Beta Agonists (e.g. Albuterol) 4-6 hours before test
- Stop Short-Acting Muscarinic Antagonists (e.g. Ipratropium Bromide) 12 hours before test
- Stop long acting beta Agonists (e.g. Salmeterol) 24 hours before test
- Stop long acting Muscarinic Antagonists (e.g. Tiotropium or Spiriva) 36 to 48 hours before test
- Avoid Tobacco for one before test
- Avoid caffeinated coffee in amount >16 oz before test
VII. Protocol: Testing
- Pulmonary Function Test (PFT)
- Adult: 15 minutes
- Child: 15-30 minutes (age 5 years and older)
- Full Pulmonary Function Test (PFT) with pre- and post-Bronchodilator testing
- Time: 45 minutes
- Full Pulmonary Function Test (PFT) and Carbon Monoxide diffusion (DLCO)
- Time: 60 minutes
VIII. Tests: Screening Spirometry Measures
- Forced Vital Capacity (FVC)
- Abnormal
- Less than lower limit of normal for adults OR
- Less than 80% of predicted for ages 5 to 18 years old
- Obstructive Lung Disease: Mildly decreased or normal
- Restrictive Lung Disease: Mildly to severely decreased
- Calculation
- FVC = Race * 1.1 * ((0.0576 * HtCm) - (0.0269 * AgeY) - 4.34)
- Where HtCm = Height in cm
- Where AgeY = Age in years
- Where Race
- Caucasian = 1
- Black = 0.87
- Asian = 0.93
- Example: 20 year old white male at height 178 cm, weight 70 kg
- FVC (L) = 1.1 * ((0.0576 * 178)-(0.0269*20)-4.34) = 5.9 L
- Abnormal
- Forced Expiratory Volume in 1 Second (FEV1)
- Maximal rate of expiration in first 1 second (recorded on spirometer)
- Patient inspires to full inspiration (Total Lung Capacity)
- Expires towards full expiration (Residual Volume)
- Interpretation
- Obstructive Lung Disease (Asthma, COPD)
- Mildly to severely decreased
- Airway obstruction slows the maximal rate of expiration, but Lung Volumes are normal (or hyperexpanded)
- Restrictive Lung Disease
- Moderately to severely decreased
- However, low FEV1 is due to low FVC (and FEV1/FVC ratio is normal)
- Obstructive Lung Disease (Asthma, COPD)
- Normal FEV1 estimation
- FEV1 = Race * 1.08 * ((0.043 * HtCm) - (0.029 * AgeY) - 2.49)
- See Legend above (under FVC)
- Example: 20 year old white male at height 178 cm, weight 70 kg
- FEV1 (L) = 1.08 * ((0.043 * 178)-(0.029*20)-2.49) = 4.95 L
- FEV1 = Race * 1.08 * ((0.043 * HtCm) - (0.029 * AgeY) - 2.49)
- Maximal rate of expiration in first 1 second (recorded on spirometer)
- FEV1 to FVC Ratio (Normally over 75%)
- Not useful if both FEV1 and FVC are normal
- Obstructive Lung Disease: Moderately to severely decreased
- Restrictive Lung Disease: Normal or increased
- COPD Gold criteria define abnormal FEV1/FVC <0.7
- Interpretation via Lower Limit of Normal (LLN) is preferred and used by ATS/ERS guidelines
- Lower limit of normal is <5th percentile for ethnicity and age
- Swanney (2008) Thorax 63:1046–51 [PubMed]
- Normal ranges vary by age
- Age 8 to 19 years: FEV1/FVC 85%
- Age 20 to 39 years: FEV1/FVC 80%
- Age 40 to 59 years: FEV1/FVC 75%
- Age 60 to 80 years: FEV1/FVC 70%
- Calculation
- FEV1 to FVC Ratio = 87.2 - (0.18 * AgeY)
- Forced Expiratory Small Airway Flow (FEF25-75)
- Effort Independent
- More variable than FEV1 or FVC
- References
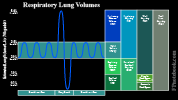
IX. Tests: Complete Lung Volume
- See Lung Volumes (includes Tidal Volume, Vital Capacity, Residual Volume and Functional Residual Capacity)
-
Total Lung Capacity (TLC)
- Obstructive Lung Disease: Normal or mild change
- Restrictive Lung Disease: Decreased
-
Residual Volume (RV)
- Residual Volume is not directly measured by Spirometry
- Functional Residual Capacity (FRC) is measured by plethysmography, gas dilution (e.g. helium) or nitrogen washout
- Expiratory Reserve Volume (ERV) is measured
- Residual Volume (RV) = FRC - ERV
- Obstructive Lung Disease: Increased
- Restrictive Lung Disease: Decreased
- Residual Volume is not directly measured by Spirometry
- Maximal voluntary ventilation (MMV)
- Technique
- Patient breathes hard and fast for 12 seconds
- Calculate liters per minute by extrapolating
- Interpretation
- Normal: MMV = FEV1 x 40
- Low MMV
- FEV1 and FVC reduced: Restrictive Lung Disease
- FEV1 and FVC normal
- Inadequate effort or neuromuscular disease
- Severe airway disorder
- Technique
X. Tests: Additional
-
Diffusing Capacity (DLCO)
- Reversible Obstructive Lung Disease (Asthma): Normal
- Irreversible Obstructive Lung Disease (COPD): Low
- Inhalation Challenge Test (Methacholine Challenge)
- Lung elasticity
- Airway resistance
- Respiratory Muscle Strength (e.g. Myasthenia Gravis, Guillain Barre, ALS, Ventilator Weaning)
- Single Breath Counting
- Negative Inspiratory Flow (NIF) or Maximal Inspiratory Pressure (MIP)
- NIF less negative than -20 to -30 cmH2O may predict Respiratory Failure in Myasthenia Gravis
- NIF less negative than-25 cmH2O may predict Ventilator Weaning failure
-
Bronchodilator response (Significant values)
- Response suggests reversible component
- FVC or FEV1 improves by 12 to 15% over baseline
- FVC or FEV1 increases by at least 200 ml
- FEF25-75 improves by 15 to 25% over baseline
-
Exercise Testing Endpoints
- Patient uncomfortable and requests to stop
- Disturbing Physiologic Change
- Reaching 90% of maximum Heart Rate (age predicted)
XI. Protocol: Approach
- Step 1: Determine validity of Pulmonary Function Testing
- See Criteria above
- Step 2: Evaluate FEV1 to FVC Ratio
- FEV1 to FVC Ratio <0.7 (or <LLN or for children<85% of predicted)
- Go to Step 4 (Obstructive Lung Disease evaluation)
- FEV1 to FVC Ratio Normal
- Go to Step 3 (Restrictive Lung Disease evaluation)
- FEV1 to FVC Ratio <0.7 (or <LLN or for children<85% of predicted)
- Step 3: Restrictive Lung Disease Evaluation (FEV1 to FVC Normal)
- Forced Vital Capacity (FVC) < LLN (or for age 5 to 18 years old, <80% of predicted)
- Consistent with Restrictive Lung Disease
- Perform complete Pulmonary Function Tests with DLCO
- Consider Restrictive Lung Disease differential diagnosis
- Forced Vital Capacity (FVC) Normal
- No Restrictive Lung Disease
- Consider further Asthma Evaluation if high level of suspicion
- Forced Vital Capacity (FVC) < LLN (or for age 5 to 18 years old, <80% of predicted)
- Step 4: Obstructive Lung Disease Evaluation (FEV1 to FVC Low)
- Forced Vital Capacity (FVC) Normal
- Consistent with Obstructive Lung Disease
- Bronchodilator response with FEV1 or FVC increased >12% at any age (or >200 ml in adults)
- Consistent with reversible Obstructive Lung Disease (Asthma)
- Inadequate Bronchodilator response
- Consistent with irreversible Obstructive Lung Disease (COPD)
- Forced Vital Capacity (FVC) < LLN (or for age 5 to 18 years old, <80% of predicted)
- Consistent with mixed obstructive-Restrictive Lung Disease
- Go to Step 5
- Forced Vital Capacity (FVC) Normal
- Step 5: Mixed Obstructive-Restrictive Lung Disease (FEV1 to FVC Low and FVC decreased)
- Consistent with Mixed Obstructive Lung Disease - Restrictive Lung Disease
- Assess Bronchodilator response
- FVC increases >80% of predicted in children (or >LLN in adults) with Bronchodilator
- Suspect COPD with pure Obstructive Lung Disease and air trapping
- FVC with inadequate Bronchodilator response
- Evaluate and treat as Restrictive Lung Disease
- Perform complete Pulmonary Function Tests with DLCO
- Consider Restrictive Lung Disease differential diagnosis
- FVC increases >80% of predicted in children (or >LLN in adults) with Bronchodilator
XII. Interpretation: Flow Volume Loop
- Technique
- Patient inspires to full inspiration (Total Lung Capacity)
- Patient expires to full expiration (Residual Volume) at maximal expiratory force
- Flow (L/min) is recorded continuously on Y Axis
- Normal expiratory flow is rapid at the start in healthy patients (see FEV1)
- Volume is recorded on X Axis
-
Obstructive Lung Disease (small airway obstruction of Asthma or COPD)
- Concave bowing of the the expiratory loop
-
Restrictive Lung Disease
- Expiration time is shortened, so the curve appears narrowed on the X-axis
- Flattening of the flow volume curve
- Sub-maximal effort is most common cause
- High grade upper airway obstruction
- Maximal inspiratory flow rate <2 L/s
- Fixed large airway obstruction (tracheal stenosis, main-stem Bronchus)
- Flattening of both the inspiratory and expiratory curves
- Variable extra-thoracic large airway obstruction
- Flattening of the inspiratory curve (e.g. Vocal Cord Dysfunction)
- Flattening of the expiratory curve (e.g. tracheal cancer)
- Flow is greater during inspiration than expiration
- Trachea's posterior membrane billows outward during inspiration (increased flow)
- Airway narrows during expiration (pleural pressure > intrathoracic pressure)
XIII. Interpretation: Normal
- Forced Expiratory Volume in one second (FEV1)
- Normal
- FEV1 >80% of predicted
- Mild Obstructive Lung Disease
- FEV1 70-80% of predicted
- Moderate Obstructive Lung Disease
- FEV1 50-70% of predicted
- Severe Obstructive Lung Disease
- FEV1 <50% of predicted
- Normal
- Forced Vital Capacity (FVC)
- Adult: > Lower Limit of Normal (LLN)
- Ages 5-18 years old: >80% of predicted
- FEV1 to FVC Ratio
- Adult GOLD Criteria: >0.7
- Adult ATS Criteria: > Lower Limit of Normal (LLN)
- Ages 5-18 years old: >85% of predicted
- Lower Limit if Normal (LLN) - Used in ATS Guidelines
- Based on Third National Health and Nutrition Examination Survey (NHANES III) PFT data
- Calculated the lowest 5% (fifth percentile) cut-offs for FEV1 to FVC, FVC and FEV1
- Replaces GOLD Criteria which are less accurate
- Miss up to 50% of young adults with Obstructive Lung Disease and
- Overdiagnose Obstructive Lung Disease in healthy non-smokers
- Recently manufactured PFT software calculates the LLN based on patient age, gender and height
- Online calculator
XIV. Interpretation: Abnormal
-
Obstructive Lung Disease
- FEV1 to FVC Ratio <0.7 (or <LLN or for children<85% of predicted) AND
- Normal FVC or FVC response to Bronchodilator
- Reversible Obstructive Lung Disease (Asthma) criteria
- Bronchodilator response with FEV1 or FVC increased >12% at any age (or >200 ml in adults)
-
Restrictive Lung Disease - Interstitial Lung Disease (Low Residual Volume, low DLCO)
- FEV1 to FVC Ratio >0.7 (or >LLN or for children>85% of predicted) AND
- FVC < LLN (or for age 5 to 18 years old, <80% of predicted)
- Vital Capacity (VC) and Residual Volume (RV) are typically reduced symmetrically in Interstitial Lung Disease
-
Restrictive Lung Disease - Neuromuscular Disorders (Normal Residual Volume, normal DLCO)
- Decreased FVC
- Normal or increased Residual Volume (RV)
- Normal DLCO
- Seen with weak respiratory Muscles
- Mixed Obstructive-Restrictive Lung Disease
- Criteria
- FEV1 to FVC Ratio <0.7 (or <LLN or for children<85% of predicted) AND
- Low FVC
- Approach: Bronchodilator response
- FVC increases >80% of predicted in children (or >LLN in adults) with Bronchodilator
- Suspect COPD with pure Obstructive Lung Disease and air trapping
- FVC with inadequate Bronchodilator response
- Evaluate and treat as Restrictive Lung Disease
- FVC increases >80% of predicted in children (or >LLN in adults) with Bronchodilator
- Criteria
- Chronic Bronchitis with terminal Bronchiole scarring (Expiratory Airflow Obstruction)
-
Emphysema with destruction of peri-alevolar tissue (Airway Obstruction, Hyperinflation, decreased DLCO)
- Typically seen in combination with Chronic Bronchitis
- FEV1 to FVC Ratio <0.7
- Total Lung Capacity (TLC)>120% of predicted (hyperinflation)
- Decreased DLCO
-
Asthma (Airway Obstruction, Hyperinflation, normal DLCO)
- FEV1 to FVC Ratio <0.7
- Total Lung Capacity (TLC)>120% of predicted (hyperinflation)
- Normal DLCO
XV. Precautions
- Spirometry is a crude predictor of pre-operative condition
- Spirometry is affected by
- Pneumonia or other acute lung disease
- Sleep Apnea
- Anxiety
-
Lung Volumes vary by ethnicity
- Lung Volume is lower in Black, Asian and Native American
- These groups have 8% lower Lung Volumes than whites (on average)
XVI. Resources
- Spirometry Normal Calculator (CDC NIOSH)
XVII. References
- Crapo in Goldman (2000) Cecil Medicine, p. 382-7
- Gold in Murray and Nadel (2000) Respiratory, p. 784-90
- Barreirdo (2004) Am Fam Physician 69:1107-14 [PubMed]
- Johnson (2014) Am Fam Physician 89(5): 359-66 [PubMed]
- Langan (2020) Am Fam Physician 101(6): 362-8 [PubMed]
- Pellegrino (2005) Eur Resp J 26(5): 948-68 [PubMed]
- Salzman (1999) J Respir Dis 20:809-22 [PubMed]