II. Background
- At rest
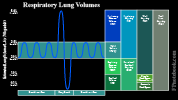
- Tidal Volume (TV) represents basal respiratory flow, in and out (similar to gentle ocean tides)
- With exertion
- Vital Capacity (IRV and ERV, in addition to TV) is recruited to allow for deeper breaths
- Analogous to Cardiac Stroke Volume, which increases with exertion
- May increase with Exercise from 500 ml to 4200 ml per breath (TV+IRV +ERV) in 70 kg adult
- In Obstructive Lung Disease (Asthma, COPD), taking deep breaths is primary compensation
- Increasing Tidal Volume with deep breaths is less work than increasing Respiratory Rate
- When Vital Capacity is insufficient to support exertion, Respiratory Rate (RR) increases
- Respiratory Rate is analogous to Heart Rate in compensation for exertion
- May increase with Exercise, from 12 to 36 breaths per minute with strenuous Exercise
- Increased Respiratory Rate is primary compensation in high lung elastic rebound
- Increasing Respiratory Rate is less energy for these patients, then taking deep breaths
- Minute Ventilation may increase with Exercise from 6 L/min to over 150 L/min
- Vital Capacity (IRV and ERV, in addition to TV) is recruited to allow for deeper breaths
- Images
III. Interpretation: Overall Lung Volumes
-
Vital Capacity (VC)
- Maximal volume expelled after maximal inspiration
- VC = ERV + TV + IRV
- VC = TLC - RV
- Decreased with low Lung Compliance, high elastic rebound (e.g. Restrictive Lung Disease, pulmonary fibrosis)
- Also low in Obstructive Lung Disease (e.g. Asthma, COPD), due to limited expiration (high Residual Volume)
- Total Lung Capacity (TLC)
- Volume in lungs at end of maximal inspiration
- Calculation: VC + RV
- Normal adult: 4-6 Liters
- Minute Ventilation (MV, Respiratory Minute Volume)
- Volume of breath inspired (and expired) per minute
- MV = TidalVolume x RespiratoryRate
- Typical resting Minute Ventilation in a 70 kg male is 6 liters/min = 500 ml TV x 12 breaths/min
- Alveolar Ventilation
- Volume of inspired air entering the alveoli per minute
- Similar to Minute Ventilation but subtracts alveolar dead space
- Aveolar dead space is 30-33% of Minute Ventilation in normal lungs (primarily Anatomic Dead Space)
- In a healthy lung, alveolar ventilation is typically two thirds of Minute Ventilation
- In very severe, end-stage COPD, alveolar ventilation may be as low as 20% of Minute Ventilation
- AV = (TidalVolume - AnatomicDeadSpace) x RespiratoryRate
- Normal adult example = (500-150) * 16 = 5600 ml
IV. Interpretation: Inspiratory Volumes
- Inspiratory Reserve Volume (IRV)
- Additional volume that could be inspired above normal inspiration (or Tidal Volume)
- Maximal inspired volume from end-tidal inspiration
- IRV may be as high as 40-43 ml/kg or 2800 ml in a 70 kg adult)
- Tidal Volume (Vt)
- Volume inspired and expired with each normal breath
- Tidal Volume is approximately one third of Vital Capacity
- Analogous to Cardiac Stroke Volume at Rest
- Minimum volume: 3 ml/kg
- Normal volume: 6-7 ml/kg (e.g. 500 ml in a 70 kg adult at rest)
- Typical ventilator Tidal Volume settings: 6-8 ml/kg
- Inspiratory Capacity (IC)
- Maximal volume inspired from resting expiratory level
- Calculation: IRV + Vt
V. Interpretation: Expiratory Volumes
- Expiratory Reserve Volume (ERV)
- Additional volume that could be expired in addition to normal exhalation (or Tidal Volume)
- Maximal expired volume from end-tidal inspiration
- Normal: 25% of Vital Capacity (up to 15 ml/kg or 1050 ml in a 70 kg adult)
-
Functional Residual Capacity (FRC)
- Volume remaining in lungs at resting expiratory level
- Resting position of the respiratory Muscles
- Balance between the opposing recoil forces of lung and chest wall
- Functional Residual Capacity (FRC) is a key point from which other Lung Volumes are measured
- Inspiratory Capacity (IC) is measured from FRC to Total Lung Capacity (TLC)
- Expiratory Reserve Volume (ERV) is measured from FRC to Residual Volume (RV)
- FRC Measurements
- Body Plethysmography or body box
- Based on Boyle's law (Product of Pressure and Volume is constant, at constant Temperature)
- Technique
- Initial pressures are measured at mouth and in airtight box at rest (volume = FRC)
- Patient pants against a closed shutter and pressures are re-measured
- Volume has decreased from FRC to Residual Volume
- Pressure has increased
- FRC = Patm x dPb/dPm
- Where Patm = atmospheric or barometric pressure
- Where dPb = change in airtight box pressure
- Where dPm = change in mouth pressure
- Nitrogen Washout
- Start by rest breathing with normal Tidal Volumes
- At, end expiration, inhaled gas changed from room air to 100% oxygen
- Total exhaled nitrogen is measured over subsequent exhalations
- Volume of gas required to contain expired nitrogen is calculated (air is 78% nitrogen)
- Helium Dilution in Closed Circuit
- Start by rest breathing with normal Tidal Volumes
- At, end expiration, inhaled gas changed from room air to 10% helium in air
- Breathing and measurements continue until measured helium concentration reaches steady state
- Expired Carbon dioxide is absorbed by soda lime
- Used oxygen is replaced in the inspired air
- Helium concentration before and after steady state are used to calculate volume of replaced gas
- Body Plethysmography or body box
- Forced Expiratory Volume in One Second (FEV1)
- Expiratory rate (FEV1) slowed by Obstructive Lung Disease (Asthma, COPD, chest masses)
- Residual Volume (RV)
- Volume remaining in lungs after maximal expiration
- Normal adult: 1.0 to 2.4 Liters
- Includes Respiratory Dead Space (anatomic and physiologic)
- Also includes healthy respiratory zone (alveoli to Bronchioles) that contribute to gas exchange
- Allows for passive CO2 and O2 diffusion in gas remaining in aveoli and Bronchioles between breaths
- Contrast with Physiologic Dead Space in diseased respiratory zone that cannot gas exchange
- RV is not measureable with standard Spirometry/PFTs
- Requires advanced testing (e.g. nitrogen washout, helium dilution, body plethysmography)
- Increased Residual Volume may also be suggested by barrel chest, hyperexpansion on CXR
VI. Interpretation: Dead Space
- Total Dead Space (Physiologic Dead Space)
- PhysiologicDeadSpace = AnatomicDeadSpace + AlveolarDeadSpace
- Anatomic Dead Space
- Volume of air within the nose, trachea and Bronchi that does not contribute to gas exchange
- Present in all patients regardless of health, representing 30-33% of Tidal Volume (e.g. 150 ml in 70 kg adult)
- Alveolar Dead Space
- Volume of air within the respiratory zone (alveoli to Bronchioles) that does not contribute to gas exchange
- In healthy patients, alveolar dead space is minimal (<5 ml)
- In diseased lung (e.g. COPD) or edematous lung (e.g. CHF, ARDS), alveolar dead space may be large
- Severe disease total dead space may be as large as 50-80% of Tidal Volume
- Ventilation-Perfusion mismatch results in some regions of lung that are over-ventilated and other underventilated
- Over-ventilated alveoli (V/Q>1) waste ventilation as blood is saturated with oxygen at a fixed maximum
- Alveolar dead space is the total excess ventilation to over-ventilated alveoli (V/Q>1)
- Measured Dead Space
VII. Resources
- Intagliata (2020) Lung Dead Space, StatPearls, Accessed 3/30/2021
VIII. References
- Rollings (1984) Facts and Formulas, McNaughton & Gunn
- Marini (1987) Respiratory Medicine, Williams & Wilkins